This word doesn’t really exist or have a true definition,
but it seems to encompass all qualities that are related to cancer.
The inherent cancer parts of cancer.
There are so many facets to cancer in general. Each kind of cancer has its own persnickety
descriptions and terminologies.
For example, I can tell someone I had cancer.
If that person asks what kind, sometimes I will respond: blood cancer.
If that someone wants to know the specific blood cancer, I
respond: Non-Hodgkins Lymphoma.
If someone wants to know the staging, I can add that it was Stage 1/e Non-Hodgkins Lymphoma.
If I really want to get detailed, I’ll throw in extra
descriptors: Stage 1/e Mediastinal
(Diffuse) Large B-Cell Non-Hodgkins Lymphoma
See? So many fancy
names and descriptions.
My oncologist did not specifically tell me the fancy
terminology outside of Stage 1/e Non-Hodgkins Lymphoma. It’s possible that he didn’t feel the need to
be that specific. I found out the information
in pieces by gazing at my medical records, conversations with doctors at my
oncology office and those at MD Anderson, and of course research.
As a future librarian, I’m part of a group of people that
will venture forth with the following philosophy: knowledge is power. It’s pretty much ingrained in the ideology of
librarianship, but even outside of librarianship, it’s a giant dose of truth.
However, I have one piece of advice about personal research
regarding medicine: take it with a grain of salt.
It’s incredibly easy to be caught up with WebMD, anything
produced by the National Institutes of Health (NIH), and the millions of forums
and blogs out in cyberspace.
All of it will scare the crap out of you.
I mean this with no sense of irony as I write a
cancer-related blog. I mean this in
complete sincerity.
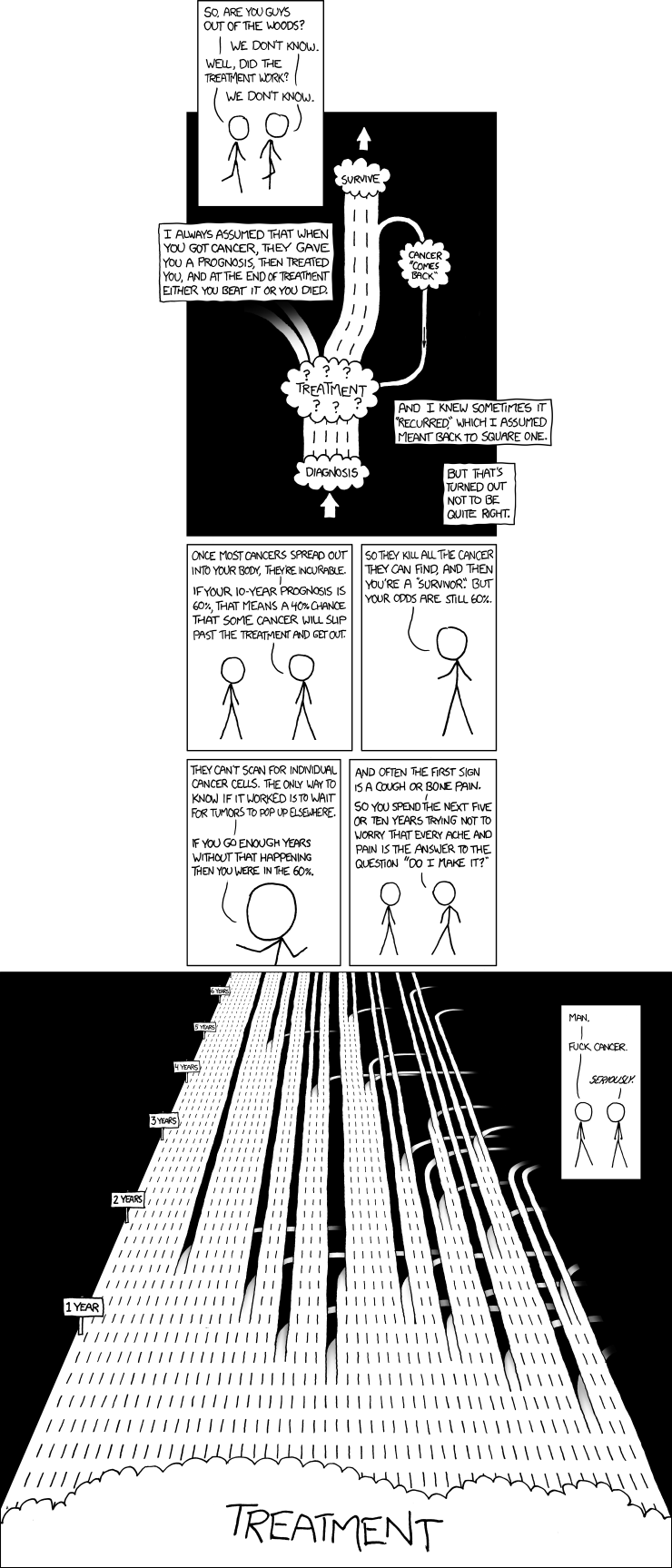
When I was first diagnosed, I gleaned as many information
sources I could find concerning cancer statistics, especially ones concerning
survival rates.
What a mind fuck.
The precious lucid moments I had between treatments
shouldn’t have been concentrating on using my graduate student access to research
academic versions of Medline databases at my university’s library in order to find
prognosis statistics.
I do believe it is empowering to use information sources to
understand cancer causes, symptoms, and treatments.
This might be a philosophy encouraged for doctors as well
since my doctor even gave me a printout from PubMed Health about Non-Hodgkins
Lymphoma during my diagnosis*.
However, to understand medical research is like opening the
server room at any IT department: a lot of friggin’ wires.
I understand this even more since I have been undertaking an
Evaluating Information Services course
this past semester.
For example, I found out there is a whole code of ethics for
research. I think on some shallow level,
I understood this, but one look at this report will tell you that there is no
fooling around:
Aside from approaching a project ethically, one has to take
into consideration the following: previous research (i.e. undertaking enough
reading to make your eyeballs bleed), various research models (i.e. make it so
complicated that no one understands what the hell you are studying), and
statistical analysis.
Statistical
analysis.
It sounds like a root canal would be more fun, right?
The permutations that can result from various data collected
seem innumerable. If you truly look at
data and apply statistical methods to analyze it, there is the possibility that
there are no correlations or too many correlations between data sets.
Considering these concepts in retrospect is illuminating
when it comes to understanding cancer research and statistics. Discovering correlations takes time and
skill. Then to disseminate all the
information to a hungry public eager to learn about their potential longevity
in the face of treatment is an equally difficult task.
It is humbling how carefully these types of research take
place. It is overwhelming to think that
there are so many pieces to take into consideration.
Enough to make me want to shut the hell up about the negative
issues with cancer research.
So, one big thought that I’ve been working through these
past few years post-treatment:
Take it one day at a time, or better yet, one minute at a
time.
Suffering over what could be or what will come next is not a
good solution. I have experience with
this. Before going through biopsy
surgery in August 2011, I tired out my chemo-ridden self with worry:
What if it is still
malignant? I will have to go UT
Southwestern and do a stem cell transplant.
What the hell is a stem cell anyways?
I will live in a bubble and no one will be allowed to visit me. My cats will steer clear of me because I will
have done the human equivalent of “control-alt-delete” and smell weird.
And so forth.
Death was also a consideration. Death tends to swagger around everything we
do as people. The finality of it is
heartbreaking (which is an understatement in itself).
In reviewing survival rates for Non-Hodgkins Lymphoma, the
statistics were, I’ll be honest, a bit grim in some areas, but most positive in
others.
I recently completed a Light the Night walk for the Leukemia
& Lymphoma Society (LLS) in October.
There were different balloons that the walkers could carry depending on
their level of support. Red balloons
went to people who were just plain supporting.
White balloons went to current patients and survivors. Gold balloons went to people who were walking
in memory of someone.
There were a lot of gold balloons during that walk.
The image began to alter as the walk ran out of red balloons
and began handing out white and gold balloons instead, but the initial image of
arriving to the walk comprehending this meaning was tear inducing.
It made me more appreciative of how well I was doing,
despite the annoying little post-treatment symptoms.
Coming back to the biopsy surgery, I recall having to start
the process of training myself not to get too far ahead mentally.
My mind would wander: tomorrow
is my surgery…wait, what am I doing
now? I am cooking. I will concentrate on the boiling water and
pull out the necessary utensils to finish cooking. Hmm, those knives sure are sharp. I wonder if there will be sharp knives used
for tomorrow’s…ok, shut up. You are
boiling water.
I’m learning that this takes practice and cancerness is a
lesson in patience.
Moments are singular pieces of time and moments stacked up are life.
I urge you to look at the moments.
*Note: I just noticed
recently from the URL at the bottom of the printout that was given to me that
the page was last updated in February 2013.
It’s interesting to see the evolution**.
**Additional note:
from a research perspective, it’s beneficial to refer to sources that update
regularly. Otherwise, you might not be
getting factual or up-to-date information.
Just some friendly librarian advice.